ECHINOCOCCOSIS ( HYDATID DISEASE)
Hydatid disease is caused by larvae of the platyhelminth parasite called Echinococcus; it generally lodges in the liver and lung, and less commonly in spleen. There are two species of the genus Echinococcus, Echinococcus multilocularis (also called alveolar hydatid) and Echinococcus granulosus, characterized by distinct growth features in humans. The main endemic regions for human alveolar echinococcos is caused by Echinococcus. Multilocularis are Central Europe, Russia, Turkey, Japan, China, eastern France and North America. Human echinococcosis is usually caused by an intrahepatic growth of parasitic larvae. Cerebral occurrence of E. multilocularis disease is rare, accounting for only 1% of cases, and is generally considered to be fatal.
Etiology and pathogenesis. Echinococcosis, or hydatidosis, is one of the most important zoonoses.
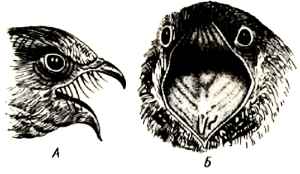
The species Echinococcus granulosus is the cause of cystic hydatid disease, the hydatid disease most commonly seen throughout the world. Areas of high incidence include East Africa, Spain, Greece, the Middle East, Iran. E. multilocularis causes alveolar hydatid disease that is seen mostly in Alaska, Canada and central Europe. The definitive hosts for the adult cestode are commonly the domestic dog for E. granulosus and the fox for E. multilocularis.
The adult tapeworms, which may number several thousands in the heavily infected dog intestine, shed both eggs and gravid proglottids, which can be found in the host's stool. Human and the natural intermediate hosts become infected when they swallow these immediately infective eggs. In the duodenum the larvae or oncospheres are freed and, using their hooklets, find their way through the intestinal mucosa into the lumen of blood vessels. They are then carried by the blood until they lodge in capillaries at almost any site. In 60% of cases, the larvae are retained in the sinusoids of the liver. The remainder pass through the hepatic circulation, and 20% are retained in the lung; the others gain access to the systemic circulation.
Morphology. The cysts have an outer laminated, elastic layer and an inner germinal layer. They enlarge gradually for several months until they attain a diameter of 10 to 20 cm. Abundant clear fluid is contained within the cysts. The germinal layer develops numerous papillae, which become pedunculated vesicles containing scolices. Cysts of echinococcosis occur more frequently in the liver or in the lung.
The cysts may become secondarily infected, suppurate, and produce the clinical picture of hepatic abscess. Some of the cysts may collapse and undergo fibrosis and, not infrequently, calcification.
In E. multilocularis, the daughter cysts, which arise from the germinal membrane by budding, develop on the outside of the original (mother) cyst. This results in invasion of surrounding parenchyma by the new scolices, which are not contained by the laminated cuticular membrane.
The complications are connected with hepatic failure, amyloidosis may develop.
ASCARIASIS
Etiology and pathogenesis. Ascaris lumbricoides is a nematode of worldwide distribution, most prevalent in tropical and subtropical countries. The incidence and severity of the infection are closely related to hygienic levels. The adult worms range from 15 to 30 cm in length and from 3 to 5 mm in diameter. The minimum weight of a worm producing eggs is 1.1 g. On average, the number of eggs produced by the female decrease with increase in the worm load.
The eggs are deposited in the soil, where they undergo a period of incubation. The infection is acquired by ingestion of the fully embryonated ova. The larvae are hatched in the small intestine and penetrate the wall, reaching the lungs by way of
venules or lymphatics. They pass into the alveoli from the alveolar capillaries and migrate up the main bronchial tree and down the esophagus with the swallowed saliva. In the small intestine they grow into adult males or females.
Morphology. Frequently anteroventral pneumonia, atrophic rhinitis, and liver lesions develop. Severe cholangitis has been the main finding, but other changes has also been detected, such as pyloric and intestinal metaplasia, hyperplasia of the epithelial lining, with intraductal papillomas and adenomatous proliferation. Remnants of the worm are observed tightly adhered to the epithelium, forming microscopic intrahepatic calculi. Mucopolysaccharides, especially acid, show to be strongly positive on the luminal border, and in proliferated glands around the ducts.
Characteristic signs of biliary ascariasis are, in the longitudinal section, the «strip sign», «spaghetti sign», «inner tube sign». The helminth can travel from out of the biliary duct system back into the intestines, so that control examinations can even be negative.
Ascariasis is usually a benign and self-limited disease because of the short life span of the adult worm (6 to 12 months). The most frequent complications of ascariasis are caused by the adult parasite. Large masses of worms may produce intestinal obstruction, appendicitis, perforation and perinonitis.
SYPHILIS
Several years ago it looked as if we were on the brink of eliminating syphilis over the world. For instance, two decades of data demonstrated a consistent, downward trend in the number of reported cases, with overall rates of infectious syphilis in Canada remaining stable between 1993 and 1996, at about 0.5 per 100 000. The only change over this 4-year window was in the age distribution of incident cases. In contrast to previous years, in 1996 syphilis rates were highest among men and women 25—29 years old. At that time it was impossible to draw conclusions from this change; however, the implications have subsequently declared themselves through local resurgence in sexually active populations. The projected overall 2001 rate in Canada rose sharply to 0.9 per 100 OOO.The rate is increasing among both men and women.
In 1995, the incidence of syphilis in Russia was 86 times higher (172/100000) than in Finland (2/100,000) and is increasing (twofold during 1994— 95). In 1995,255,000 cases of syphilis were reported in the Russian Federation.
After declining every year since 1990, the number of reported cases of syphilis increased slightly in 2001.
In 2000, the rate of syphilis in the United States declined to 2.1 cases per 100,000 population, the lowest rate since reporting began in 1941. In 2001, the rate of syphilis increased slightly, to 2.2, the first annual rate increase since 1990, and 6,103 cases of syphilis were reported, a 2.1% increase in reported cases compared with 2000. In 2001, rates of syphilis were 114.3% higher for men than for women. During 2000—2001, the rate increased 15.4% among men and decreased 17.6% among women.
Syphilis is caused by a spirochaete, Treponema pallidum, which is mainly transmitted through sexual contact. The organisms gain access at the site of inoculation, usually the genitalia, and produce the primary lesion, known as a chancre. The organism is then disseminated throughout many organs from the site of inoculation. Syphilis causes chronic inflammation with type IV hypersensitivity.
An immune response develops and the primary infection heals but, thereafter, the disease becomes a chronic inflammatory condition, affecting many organs. Serological tests can be performed to detect infection.
The pattern of disease is usually divided into four stages:
1 Primary syphilis.
2 Secondary syphilis.
3 Latent syphilis.
4 Tertiary syphilis.
Primary syphilis. A chronic inflammatory nodule (chancre) forms in the skin or mucosa at the site of entry of the organism (typically penis, vulva or cervix). There is a heavy infiltrate of chronic inflammatory cells, particularly lymphocytes and plasma cells, which develops 1—12 weeks after exposure. The chancre ulcerates and there may be painless enlargement of local lymph nodes. Many spirochaetes are present in the chancre, which is highly infectious. Long before the primary lesion develops, organisms have migrated to regional lymph nodes and throughout the body via the bloodstream. Frequently, the primary lesion is not noticed by the patient.
Secondary syphilis. This stage typically occurs 1—3 months after onset of the infection, resulting from spread of the organism to many sites in the body. The most obvious manifestations are: any of a number of skin rashes (most frequently a coppery brown, diffuse, macular rash); mucosal involvement, with the formation of ulceration in the buccal mucosa (snail-track ulcers); shallow ulcers in the genital mucosa; and, often, the formation of warty growths around the genitalia (condylomata lata). Not only is this secondary stage the most infective, with large numbers of organisms in the ulcerated and warty mucosal lesions, the organism is also most likely to be transmitted to another person at this point.
Generalized enlargement of the lymph nodes may also occur, and organisms are numerous in the lymph nodes. This stage typically lasts A—12 weeks.
The lymphadenopathy of syphilis usually affects the inguinal nodes, but generalized adenopathy may be present in secondary syphilis. Microscopically capsular inflammation and fibrosis are found. The architecture of the nodes is preserved, and follicular centers are very active. Plasmacytosis is noted in the interfollicular areas and capsule. Necrotizing granulomas may be seen. Spirochetes may be demonstrated by silver stain.
Latent syphilis. This is a stage in which an infected person is asymptomatic but still harbours the infection. There may be recurrence of secondary syphilis during this period.
Tertiary syphilis. This occurs after a period of latency, typically after 3—30 years. It affects about one-third of patients who have untreated syphilis.
There are two main histological patterns of disease:
• Small vessels develop proliferation of their intimal lining, with surrounding plasma cell infiltration (endarteritis obliterans). This leads to tissue damage because of poor blood supply. The main consequence is development of thoracic aortic aneurysm.
• A Type IV cell-mediated immune response causes areas of necrosis to develop in several tissues. These areas of necrosis, known as «gummas», are surrounded by activated macrophages, fibroblasts, and lymphoid cells including plasma cells.
Neurosyphilis is one of tertiary syphilis. There are sevelal forms of neurosyphilis. Meningovascular syphilis, which may occur a few years after initial
infection, is characterized by syphilitic arteritis in association with meningitis. The neural parenchyma may be involved secondarily.
Macroscopically a yellow opaque exudate is found in the meninges, at times containing tiny, firm nodules. Microscopically, there is infiltration of the subarachnoid space and pia mater by plasma cells and lymphocytes, followed by extension of the exudate into the perivascular spaces of the superficial parenchyma. Proliferation of fibroblasts and capillaries gives rise to syphilitic granulomas (gummas). Spirochetes are rarely demonstrable in the leptomeninges and blood vessel walls.
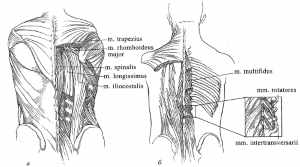
Parenchymatous syphilis. Tabes dorsalis typically begins 8 to 12 years after initial infection, most often in men in the fourth and fifth decades of life. About 2% to 3% of persons with syphilis develop tabes.
Pathology. The posterior columns of the spinal cord are reduced in size. Microscopic examination in the early stages shows localized changes around the dorsal roots in the lumbar region, with granulation tissue formation as occurs in meningovascular syphilis. Spirochetes are present in these radicular leptome-ningeal sheaths. Degeneration of axons and myelin sheaths in the dorsal roots also occurs.
Syphilitic heart disease devepops at tertiary syphilis. Although myocardial gummas may be associated with cardiac dysfunction in rare cases, syphilitic carditis usually is a complication of the much more common syphilitic aortitis.
Obliterative endarteritis of the vasa vasorum, particularly of the ascending portion of the thoracic aorta, leads to ischemic medial necrosis and fibrosis of the media and adventitia. Secondary atherosclerosis adds to the injury, which results in the formation of a thoracic aortic aneurysm.
Proximal extension of this process leads to scarring and dilatation of the aortic valve ring fibrosis of the valve leaflets, and narrowing of the coronary ostia. The resultant aortic insufficiency may lead to massive dilatation and hypertrophy of the left ventricle, with the weight of the heart being as much as 1000 g.
Congenital syphilis is the result of transmission of the organism from an affected pregnant mother to the fetus, and many fetuses are stillborn as a result. Transmission does not occur before the fifth month of gestation.
Depending on the magnitude of the infection, the fetus may die in utero or soon after birth, or it may survive. In this case infant shows a spread, fulminant infection, with spirochetemia, that differs from any of the classic stages of acquired syphilis.
The most striking injuries affect the mucocutaneous surfaces and the bones. A diffuse macu-lopapular rash develops, which differs from that of acquired syphilis by tendency to cause extensive desquamation of the skin. A generalized osteochondritis and perichondratis are present. Destruction of the vomer of the nose produces the characteristic
saddle deformity; inflammatory proliferation of the anterior surface of the tibiae causes the typical anterior bowing or sabre shins; and dental malformations create wedge-shaped notched incisors and «mulberry molars». A diffuse interstitial inflammatory reaction with prominent sclerosis affect any organ of the body. In particular, the liver and lungs are usually involved, with syphilitic hepatitis, syphilitic pneumonia development.
The eyes commonly show an interstitial keratitis or a choroiditis, and sometimes areas of abnormal pigmentation of the retinae.
Imunohistochemical method may be used at pathologic anatomy diagnosis. Tissue from the gastrointestinal tract, brain, liver, spleen, and lung is studied by using direct fluorescent antibody and immunohistochemical analysis (IHC) for Treponema pallidum. The inflammatory infiltrate is characterized by using IHC against CD3, CD20, CD68, and smooth muscle actin. The diagnosis of congenital syphilis is confirmed by demonstrating spirochetes in tissues with IHC and direct fluorescent antibody examination. IHC showed abundant treponemes in the small intestine and liver and occasional spirochetes in the meninges. Bacteria are seen as intact spirochetes, granular staining, or large extracellular collections of antigen. A constant pathologic feature throughout the tissues is concentric macrophage (CD68-positive) infiltrate around vessels, giving an onion-skin appearance.
Дата добавления: 2016-07-27; просмотров: 1639;