Questions to control the knowledge
1. Which the most frequent way of diphtheritic infection do you know?
2. In what form of diphtheria is the most evident intoxication of the body observed and why?
3. What changes in the heart may cause death in the early and late periods of diphtheria?
4. List the most frequent complications of diphtheria from the side of the nervous system and adrenal glands.
5. Specify the notions of the «laryngeal diphtheria» and «descending croup» in diphtheria.
6. Give the definition of scarlet fever. What do «flaming fauces» and «strawberry tongue» mean?
7. What kind of inflammation in the fauces is typical for the septic form of scarlet fever?
8. List the most typical changes in the kidneys which develop during the second period of scarlet fever.
9. Which complications of the first period of scarlet fever do you know?
10. Describe the character of rash and desquamation in scarlet fever.
11. Name the infection atrium of the measles virus.
12. What changes develop in the upper respiratory tract in uncomplicated measles?
13. What causes development of complications in measles?
14. Explain the clinical-epidemiological significance of meningococcal carriage and meningococcal nasopharyngitis.
15. Specify the notion of «Waterhouse-Friderichsen syndrome». When does this syndrome develop in meningococcal infection?
16. Describe the mechanism of development of hydrocephaly in meningitis.
17. List complications and outcomes of meningococcal meningitis.
18. Describe changes in the upper respiratory tract in whooping cough.
19. Describe the mechanism of the «respiratory tract neurosis» in whooping cough.
20. List complications and causes of death in whooping cough.
Terminology:
Diphtheria, Waterhouse-Friderichsen syndrome, scarlet fever; «flaming fauces»; «strawberry tongue», rash (exanthema), laminar desquamation; retropharyngeal abscess, meningococcal infection, meningitis, meningococcemia, measles, whooping cough, apnea, asphyxia.
TUBERCULOSIS
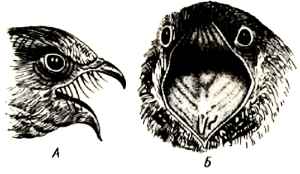
Etiology. Tuberculosis is a classical chronic specific granulomatous inflammation caused by Mycobacterium tuberculosis or Koch's bacillus. R. Koch discovered this basillus in 1882. The organism has 5 distinct pathogenic strains: hominis, bovis, avium, murine, and cold-blooded vertebrate strain. The first two strains (hominis and bovis) are definitely infective to people. There are 4 groups of atypical mycobacteria: photochromogens, scotochromogens, non-chromogens and rapid growers. M. tuberculosis hominis is a slender rod-like bacillus, 4 μm in length, and can be demonstrated by the following methods: Acid fast staining, fluorescent dye methods, culture of the organism in Lowenstein-Jensen medium for 6 weeks, Guinea pig inoculation method by subcutaneous injection of the organisms.
In spite of great advances in chemotherapy and immunology, tuberculosis still continues to be worldwide in distribution, more common in developing countries of Africa, Latin America and Asia.
Epidemiology. Human beings acquire infection with tubercle bacilli by one of the following routes:
• inhalation of organisms present in fresh cough droplets or in dried sputum from an open case of pulmonary tuberculosis;
• ingestion of the organisms leads to development to tonsillar or intestinal tuberculosis. This mode of infection of human tubercle bacilli is from self-swallowing of infected sputum of an open case of pulmonary tuberculosis, or ingestion of bovine tubercle bacilli from milk of diseased cows;
• inoculation of the organisms into the skin may rarely occur from infected postmortem tissue;
• transplacental route results in development of congenital tuberculosis in fetus from infected mother and is a rare mode of transmission.
The disease spreads in the body by various routes:
1. Local spread. This takes place by macrophages carrying the bacilli into the surrounding tissues.
2. Lymphatic spread. Tuberculosis is primarily an infection of lymphoid tissues. The bacilli may pass into lymphoid follicles of pharynx, bronchi, intestines or regional lymph nodes resulting in regional tuberculous lymphadenitis which is typical of childhood infections. Primary complex is primary focus with lymphangitis and lymphadenitis.
3. Hematogenous spread. This occurs either as a result of tuberculous bacillemia because of the drainage of lymphatics into the venous system or due to caseous material escaping through ulcerated wall of a vein. This produces millet seed-sized lesions in
different organs of the body like lungs, liver, kidneys, bones and other tissues and is known as miliary tuberculosis.
Classification of tuberculosis.Tuberculosis is classified according to the clinical course into: tuberculosis of children and teenagers, tuberculosis of the lungs, tuberculosis of the other organs and systems.
There are 3 clinico-morphological types of tuberculosis:
1. Primary tuberculosis.
2. Secondary tuberculosis.
3. Hematogenic tuberculosis.
The most common pattern of human tuberculosis (TB) is pulmonary. The tuberculosis organism is inhaled into the alveolar spaces of the lung, but other tissues are also affected.
The main morphological characteristicof tuberculous is granuloma (tubercle) formation in the affected areas. Each tubercle has an area of caseous tissue necrosis at its center. This is characterized by its homogeneity, and no ghost pattern of the original tissue structure remains. Viable mycobacteria are present within the necrotic debris. Macroscopically, this necrotic tissue resembles cream cheese, hence its descriptive name caseous necrosis. The reason for the necrosis at the center of tubercles is uncertain, as it is not seen in the center of granulomas caused by other agents. A tubercle is composed of activated macrophages with surrounding lymphoid cells and fibroblasts.
The structure of a typical tuberculous granuloma is as follows: around the central area of caseous necrosis lies a collection of large, activated macrophages. Histologically, this functional activation is manifest by the presence of bulky pale-staining granular cytoplasm, which is rich in endoplasmic reticulum. Because of a minimal resemblance to some epithelial cells, the term epithelioid cells was originally coined for these macrophages. Some of the activated macrophages cells fuse to form large multinucleate cells with many nuclei arranged around the periphery, and a large central cytoplasmic mass. In TB these giant macrophages are called Langhans' cells. Around the zone of macrophages bordering the central caseous necrosis lies a collar of lymphocytes, reflecting the immunological response to the presence of mycobacteria.
As the tubercle persists, some fibroblasts appear within the lymphocyte collar and outside it. These are recruited by secretion of cytokines from the activated macrophages.
The outcome of tubercle formation depends on the balance between two conflicting sets of factors: those predisposing to extension of infection (ingestion of large numbers of highly virulent organisms, poor immune response) and those predisposing to containment, or healing and eradication of infection (ingestion of small numbers of poorly virulent organisms, good immune response, administration of appropriate antibiotics).
The outcomes of a granuloma may be :
1. The caseous material may undergo liquefaction and extend into surrounding soft tissues, discharging the contents on the surface. This is called cold abscess although there are no pus cells in it.
2. In tuberculosis of bones, joints, lymphnodes and epididymis, sinuses are formed and the sinus tracts are lined with tuberculous granulation tissue.
3. The adjacent granulomas may coalesce together enlarging the lesion which is surrounded by progressive fibrosis.
4. In granuloma enclosed by fibrous tissue, calcium salts may get deposited in the caseous material (dystrophic calcification) and sometimes the lesion may even get ossified over the years.
Primary tuberculosis.The infection of an individual who has not been previously infected or immunized is called primary tuberculosis or Ghon's complex, or childhood tuberculosis.
Primary complex is the lesion produced at the site of entry with foci in main draining lymphatic vessels and lymph nodes. The most commonly involved tissues for primary complex are lungs and hilar lymph nodes. The other tissues which may show primary complex are tonsils and cervical lymph nodes, and in the case of ingested bacilli the lesions may be found in small intestine and mesenteric lymph nodes.
Primary complex in lungs consists of 3 components:
Pulmonary component Lesion in the lung is the primary focus. It is 1—2 cm solitary area of tuberculous pneumonia located under the pleura, just above or just below the interlobular fissure between the upper and lower lobes of lung. Microscopically, the lung lesion consists of tuberculous granulomas with caseation necrosis.
Lymphatic vessel component The lymphatics draining the lung lesion contain phagocytes containing bacilli and may cause beaded, miliary tubercles along the path of hilar lymphnodes.
Lymphnode component. This consists of enlarged hilar and tracheo-bronchial lymph nodes in the area drained. The affected lymph nodes are matted and show caseation necrosis. Microscopically, the lesions are characterized by extensive caseation, tuberculous granulomas and fibrosis. Nodal lesions are potential source of re-infection later.
In the case of primary tuberculosis of alimentary tract due to ingestion of tubercle bacilli, a small primary focus is seen in the intestine with enlarged mesenteric lymphnodes producing tabes mesenterica. The enlarged and caseous mesenteric lymphnodes may rupture into peritoneal cavity and cause tuberculous peritonitis.
Primary complex may have one of the following outcomes: a) the lesions of primary tuberculosis of lung commonly do not progress but instead heal by fibrosis, and in time undergo calcification and even
ossification; b) in some cases, the primary focus in the lung continues to grow and the caseous material is disseminated through bronchi to the other parts of the same lung or the opposite lung. This is called progressive primary tuberculosis; c) at times, the bacilli may enter the circulation through erosion in a blood vessel and spread to various tissues and organs. This is called primary miliary tuberculosis and the lesions are seen in organs like liver, spleen, kidney, brain and bone marrow; d) in certain circumstances like in lowered resistance and increased hypersensitivity of the host, the healed lesions of primary tuberculosis may get reactivated. The bacilli lying dormant in acellular caseous material are activated and cause progressive secondary tuberculosis. It affects children more commonly but adults may also develop this kind of progression.
Secondary tuberculosis.The infection of an individual who has been previously infected or sensitized is called secondary, or post-primary or reinfection or chronic tuberculosis. The infection may be acquired from: endogenous source such as reactivation of dormant primary complex; or exogenous source such as fresh dose of re-infection by the tubercle bacilli.
Secondary tuberculosis occurs most commonly in lungs. Other sites and tissues which can be involved are tonsils, pharynx, larynx, small intestine and skin.
Secondary pulmonary tuberculosis. The lesions in secondary pulmonary tuberculosis are usually located at the subapical region of one or both the lungs, probably due to spread of infection from Simon's focus. Simon's focus is hematogenous spread of infection from primary complex to the apex of the affected lung where the oxygen tension is high and favorable for growth of aerobic tubercle bacilli.
The secondary pulmonary tuberculous lesion is located in the apex of one or both lungs. It begins as a small focus of consolidation, usually less than 3 cm in diameter, it is often called an Assmann's focus or Abrikosov's focus. An apical lesion begins as a small caseating tuberculous granuloma. Histologically similar to the Ghon's focus, it has a central area of caseous necrosis that is surrounded by a granulomatous inflammatory response. In most cases, destruction of lung leads to cavitation. There is little involvement of lymph nodes, as spread of organisms to regional nodes is prevented by a vigorous tissue-based hypersensitivity response.
There are several clinico-morphological forms (stages) of secondary pulmonary tuberculosis:
1. Acute focal tuberculosis.
2. Fibrofocal tuberculosis.
3. Infiltrative tuberculosis.
4. Tuberculoma.
5. Tuberculous caseous pneumonia.
6. Acute cavernous tuberculosis.
7. Fibrocavernous tuberculosis.
8. Cirrhotic tuberculosis.
Tuberculoma is typically a firm, lobulated mass of granulomatous inflammation with central caseous necrosis, up to several centimeters in diameter, and walled off by fibrous tissue. Lesions occur within the pulmonary parenchyma.
Fibrocavernous tuberculosis. The original area of tuberculous pneumonia undergoes massive central caseation necrosis which may: either break into a bronchus from a cavity (cavitary or open fibrocaseous tuberculosis), or remain as a soft caseous lesion without drainage into a bronchus or bronchiole to produce a non-cavitary lesion (chronic fibrocaseous tuberculosis). The cavity provides favorable environment for proliferation of tubercle bacilli due to high oxygen tension. The cavity may communicate with bronchial tree and become the source of spread of infection («open tuberculosis»). The open case of secondary tuberculosis may implant tuberculous lesion on the mucosal lining of air passages producing endobronchial and endotracheal tuberculosis. Ingestion of sputum containing tubercle bacilli from endogenous pulmonary lesions may produce laryngeal and intestinal tuberculosis.
Macroscopically, the tuberculous cavity is spherical with thick fibrous wall, lined by yellow, caseous necrotic tissue and the lumen is traversed by thrombosed blood vessels. There are foci of connective tissue growth around the wall of the cavity.
Tuberculous caseous pneumonia. In a highly susceptible, highly sensitized individual, tuberculous infection may spread rapidly throughout large areas of lung parenchyma and produce a diffuse bronchopneumonia, or lobar exudative consolidation, at one time descriptively referred to as «galloping consumption)). Sometimes, with such overwhelming disease, well-developed tubercles do not form, and it may be difficult to establish on histologic grounds the tuberculous nature of the pneumonic process. However, numerous bacilli are usually present in such exudates. Microscopically, the lesions show exudative reaction with edema, fibrin, polymorphs and monocytes but numerous tubercle bacilli can be demonstrated in the exudates.
Hematogenic tuberculosis.This is hematogenous spread of tuberculous infection from primary focus or later stages of tuberculosis. The spread is either by entry of infection into pulmonary vein producing disseminated or isolated organ lesion in different extra-pulmonary sites (e.g. liver, spleen, kidney, brain and bone marrow) or into pulmonary artery restricting the development of miliary lesions within the lung.
Sometimes, only small numbers of tubercle bacilli escape into the blood and, if host defenses are effective, most of the organisms die. However, for reasons that are not yet certain, some bacilli settle in specific organs and may remain dormant for many years, only
proliferating and producing overt disease at a later date, often after the initial lung and lymph node lesions have healed. Known as metastatic tuberculosis or isolated organ tuberculosis, those organs particularly involved in this pattern of disease include: adrenal glands, kidney, fallopian tube, epididymis, brain and meninges and bones and joints.
The main hematogenic form of tuberculosis is miliary tuberculosis of the lungs.
Miliary tuberculosis of the lungs. The miliary lesions are millet seed-sized (1 mm in diameter), yellowish, firm areas without grossly visible caseation necrosis.
Microscopically, the lesions show the structure of tubercles with minute areas of caseation necrosis.
The common non-pulmonary tuberculosis are tuberculosis of brain, kidney, bones and cartilages.
Tuberculosis of the brain. Infection of the nervous system with TB may cause meningitis or abscess. Infection of the CNS by Mycobacterium tuberculosis is by blood spread from a site of primary infection, most commonly the lung. There are two main types of infection.
Meningitis is characterized by numerous granulomas in the leptomeninges, with features of chronic meningitis. Infection is most marked around the base of the brain and, even when infection is treated, there is often development of meningeal fibrosis to cause hydrocephalus.
Tuberculous abscess (tuberculoma) forms with infection of the brain parenchyma. A tuberculoma is typically a firm, lobulated mass of granulomatous inflammation with central caseous necrosis, up to several centimeters in diameter, and walled off by fibrous tissue. Lesions occur within the cerebral hemispheres, but are most common in the cerebellum. Treatment with antibiotics is usually ineffective and surgical excision is required.
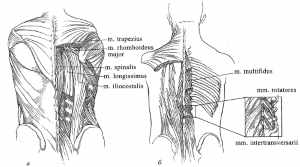
In tuberculosis of bones and cartilages tuberculous osteomyelitis — especially spondylitis, coxitis (hip joint disease), gonitis develop.
Complications of tuberculosis are variable and depend on clinico-morphological types of the disease.
In primary tuberculosis, tuberculous meningitis, pleurisy, pericarditis, peritonitis may occur.
In secondary tuberculosis, hemorrhages, pneumothorax, empyema of the pleura, amyloidosis develop.
Causes of death are cardiopulmonary insufficiency, pulmonary hemorrhage, sepsis due to disseminated miliary tuberculous, amyloidosis.
Дата добавления: 2016-07-27; просмотров: 1404;